Home » Medical Library » Anal Sac Adenocarcinoma
Anal Sac Adenocarcinoma
- Apr, 26, 2016
- DVSC
- Medical Library
- Comments Off on Anal Sac Adenocarcinoma
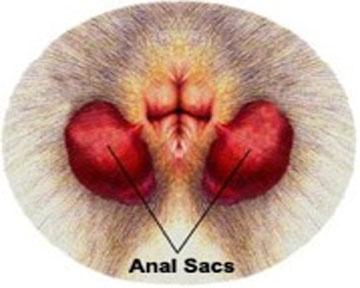
Dogs have two anal sacs (glands) beneath the skin which are located at the four and eight o’clock positions of the anus. (Figure 1) The anal sac duct opens into the edge of the anus. The anal sacs and ducts are closely associated with the anal sphincter muscle. When the anal sacs are expressed, fluid will leak from these ducts.
Apocrine gland adenocarcinoma of the anal gland is a highly malignant tumor of dogs that typically spreads to local lymph nodes and other organs in the body. Older female dogs are the most commonly affected. English Cocker Spaniels, Cavalier King Charles Spaniels, and Springer Spaniels appear to be predisposed to anal sac tumor development; however, the exact cause of anal sac cancer is not fully understood. The age at time of diagnosis is typically around 10 to 11 years, but dogs ranging from 3 to 19 years old have been diagnosed with anal sac adenocarcinoma.
Symptoms:
Early signs of anal sac disease include swelling in the site of the anal sac (Figure 2) and abnormalities when defecating (constipation, scooting, straining, or diarrhea). In 39% of dogs, anal sac tumors are found incidentally during a wellness examination with no previous signs noted. A veterinarian will perform a rectal examination to feel the anal sacs for any enlargement or irregularities; however, some anal sac tumors are very small in size and may be difficult to feel during a rectal examination. In 25% to 90% of dogs, anal sac adenocarcinoma causes elevated calcium in the bloodstream due to abnormal hormone secretions from the tumor cells. Signs of elevated calcium include increased thirst, increased frequency of urination, muscle weakness, vomiting, and constipation. Dogs with elevated calcium can also be asymptomatic.

Figure 2. Abnormal swelling in the location of the right anal sac. (Courtesy of Rita Ranch Pet Hospital)
Diagnosis:
A full bloodwork panel should be performed prior to surgery. An abdominal ultrasound and/or CT scan of the abdomen are highly recommended to check for spread of disease (metastasis), especially to the sublumbar lymph nodes. The sublumbar lymph nodes are located in the abdomen next to the aorta. Chest radiographs (x-rays) are also recommended to rule out any spread into the lungs. More than 50% of dogs will have evidence of metastasis at the time of diagnosis. The most common sites of metastasis include the sublumbar lymph nodes, lungs, liver, spleen, and bone.
Treatment:
Surgical removal of the anal sac tumor is the treatment of choice. (See Anal Sacculectomy) If spread to the sublumbar lymph nodes is suspected, surgical removal of the lymph nodes may be recommended. Additional therapies after surgery include radiation and chemotherapy, which should be discussed further with a veterinary oncologist to determine the best course of treatment after the initial surgery is performed.
Post-operative Care:
After surgery, intravenous fluids, pain medications, and antibiotics are administered in the immediate post-operative period. If the blood calcium level was high prior to surgery, it is rechecked after surgery and treated as needed. An e-collar is imperative to prevent licking at the incision site, which greatly increases the risk of infection.
Potential Complications:
Complications after anal sac tumor removal include tumor regrowth, infection, and fecal incontinence. Local tumor regrowth has been documented to occur in 29% to 45% of dogs. Infection may develop secondary to contamination from the rectum and anus. Fecal incontinence occurs in 33% of dogs and may or may not resolve with time.
Prognosis:
The prognosis is guarded for anal sac adenocarcinoma and few dogs will be cured of this disease. The average survival time is approximately 12-18 months for dogs with anal sac adenocarcinoma. Dogs that have surgery to remove the anal sac tumor will have an improved length of survival. If there is evidence of elevated blood calcium or metastatic disease prior to surgery, the survival time is typically shorter. It is important to have your veterinarian perform regular wellness examinations on your dog, including a rectal examination, to increase the likelihood of detecting anal sac tumors early in their development.
Author: Anastasia Olsen, DVM
Search This Site
Medical Library Posts
- 25+ Years of Neurosurgery at the DVSC
- Anal Sac Adenocarcinoma
- Anal Sac Removal, Elective
- Arthritis
- Arthroscopy
- Atlanto-axial (A-A) instability
- Coxofemoral (Hip) Luxation
- Cranial Cruciate Ligament (CCL) Overview
- Cranial Cruciate Ligament (CCL) – Extracapsular Repair
- Cranial Cruciate Ligament (CCL) – Tibial Plateau Leveling Osteotomy (TPLO)
- Cranial Cruciate Ligament (CCL)-Tibial Tuberosity Advancement (TTA)
- Cutaneous Mast Cell Tumors
- Cystotomy and Scrotal Urethrostomy
- Degenerative Myelopathy
- Diaphragmatic Hernia
- Diskospondylitis
- Ear Canal Ablation and Bulla Osteotomy
- Elbow Dysplasia
- Epidural Analgesia
- Episioplasty
- Feline Perineal Urethrostomy
- Femoral Head Ostectomy (FHO)
- Fibrocartilaginous Embolism (FCE)
- Fibrocartilaginous Embolus in Schnauzers
- Fracture Healing by Biologic Osteosynthesis
- Fracture of the Radius and Ulna in Small breed dogs
- Fracture Repair by Circular External Skeletal Fixator (ESF)
- Gastric Dilatation-Volvulus (Bloat)
- Gastrointestinal Foreign Body
- Gastropexy, Elective
- Hip Dysplasia (Overview)
- Hip (Coxofemoral) Luxation
- Incontinence: Urethral Sphincter Mechanism Incompetence
- The Facts About Backs (IVDD)
- Intervertebral Disc Disease (IVDD) Percutaneous Laser Disc Ablation LDA
- Intervertebral Disc Disease (IVDD)- Care of a Paralyzed Pet
- Laryngeal Paralysis
- Lumbosacral Disease
- Mandibulectomy and Maxillectomy
- Medial Patellar Luxation (MPL)
- Microvascular Dysplasia Mimics Portosystemic Shunt
- Minimally Invasive Surgery in Soft Tissue Applications
- Neurosurgical Postoperative Physical Therapy
- Perianal Fistula Management in Dogs
- Perineal Hernias
- Peritoneopercardial Hernias in Dogs and Cats
- Portosystemic Shunts
- Sialocele (Salivary Mucocele)
- Spinal Fractures and Subluxations
- Splenectomy
- Total Hip Replacement
- Tracheal Collapse
- Triple Pelvic Osteotomy (TPO)
- Underwater Treadmill
- Updates in Fracture Management
- Urethral Prolapse
- Wobblers Disease
Comments Closed