Home » Medical Library » Tracheal Collapse
Tracheal Collapse
- May, 15, 2018
- DVSC
- Medical Library, Surgery
- Comments Off on Tracheal Collapse
Background
Tracheal collapse is a chronic and progressive condition which can become life-threatening. The trachea is a tube-like structure which directs air from the mouth towards the lungs. Normally, this tube is held open by firm rings of cartilage, but with tracheal collapse these cartilage rings become weak. The weakened cartilage begins to sag allowing the trachea to narrow over time and eventually obstruct. This can occur in the portion of the trachea located in the neck, or in the portion of the trachea within the chest, or both.
Tracheal collapse is primarily a disease of middle-aged small breed dogs (Yorkshire terriers, Pomeranians, toy poodles). It is rarely diagnosed in large breed dogs. The exact cause of tracheal collapse is unknown, but evidence suggests there is likely a genetic component. Certain risk factors may include obesity, heart disease, concurrent respiratory disease, and environmental irritants (smoking, chemical cleaners, etc.).
The severity of tracheal collapse is classified into 4 grades:
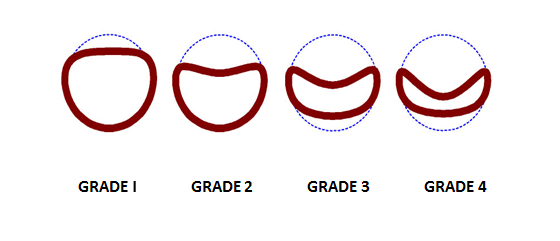
Grade 1: Lumen size is reduced by 25%
Grade 2: Lumen size is reduced by 50%
Grade 3: Cartilage is nearly flat and lumen size is reduced by 75%
Grade 4: Lumen is essentially obstructed
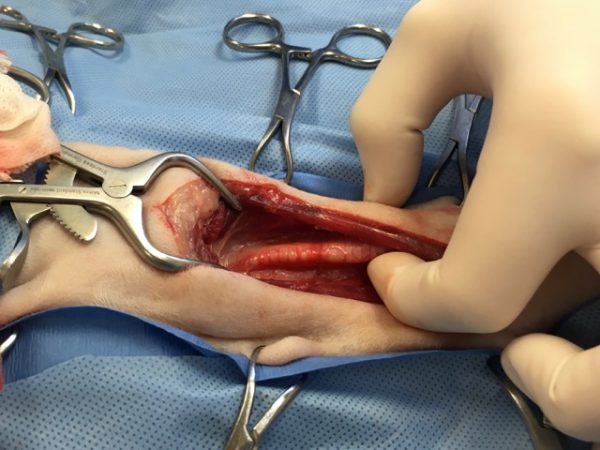
Figure 1. Intra-operative image of a grade 4 collapsed trachea. Photo courtesy of Dr. Joanne Franks, Dallas Veterinary Surgical Center
Symptoms
The signs of tracheal collapse are highly variable. Early in the disease dogs may develop an intermittent “goose honking” cough. As the disease progresses, dogs may develop exercise intolerance, shortness of breath, difficulty breathing, and experience collapse.
Diagnosis
Radiographs (x-rays) alone can often underestimate the degree of or entirely miss a diagnosis of tracheal collapse. Instead, radiographs are useful in ruling in or out diseases which can appear similar to tracheal collapse or occur in conjunction with tracheal collapse, (pneumonia, congestive heart failure, chronic bronchitis, etc.).
The key to definitively diagnosing tracheal collapse is visualizing the trachea collapsing with advanced imaging such as fluoroscopy or bronchoscopy.
Fluoroscopy is a real-time video x-ray, which is much better than plain x-rays for diagnosing tracheal collapse. When a cough is elicited, fluoroscopy can demonstrate where along the trachea the collapse is taking place, figure 2.
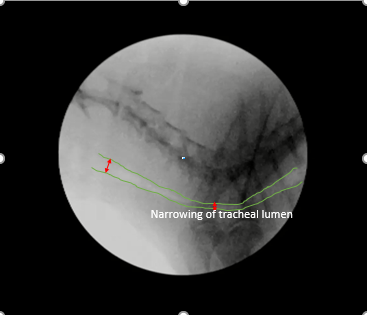
Figure 2. Fluoroscopy image identifying narrowing of the trachea. Photo courtesy of Dr. Rita Echandi, Animal Imaging
Click here to view a video demonstrating fluoroscopy of a dog with tracheal collapse.
Bronchoscopy is an imaging modality by which a camera is introduced into the trachea with the patient under anesthesia. By directly visualizing the airway, the severity and location of the tracheal collapse can be determined. If there is a concern about infection or inflammation samples can be taken during this time.
Click here to view a video demonstrating bronchoscopy of a dog with tracheal collapse.
Treatment of Tracheal Collapse
Medical Management
While there is no cure for tracheal collapse, there are several options for treatment that may improve the symptoms. Medical management is the recommended first step for all patients with tracheal collapse. The most important medical management issue for dogs with tracheal collapse is weight control. The importance of weight loss in overweight dogs with tracheal collapse cannot be over-emphasized. Weight loss is essential for successful control of this disease, to relieve pressure on the upper airway. Environments with respiratory irritants such as cigarette smoke should be avoided. A harness should be used instead of a collar.
Dogs with tracheal collapse will need lide-long medications. Steroids can be administered to help reduce airway inflammation but can have side effects including weight gain. Bronchodilators can help to expand the smaller airways to decrease mechanical irritation and improve ventilation. Antitussives are used to suppress the coughing reflex which can help break the cycle of coughing leading to increased mechanical irritation and inflammation.
Surgical Treatment
Tracheal collapse is a progressive disease and there may come a point at which weight loss and medical management fail to alleviate the symptoms. The main surgical procedures performed are the placement extraluminal prostheses (rings) or intraluminal tracheal stents. These are complex procedures which should only be performed by experienced surgeons. These surgeries are considered only for critical or high-grade tracheal collapse patients experiencing episodes of cyanosis, difficulty breathing, or syncope.
Tracheal Ring Surgery:
Extraluminal tracheal rings are made of polypropylene and designed to fit around the outside of the trachea. They are slightly larger in diameter than the trachea so that when the rings are sutured to the outside of the trachea they pull the airway open.


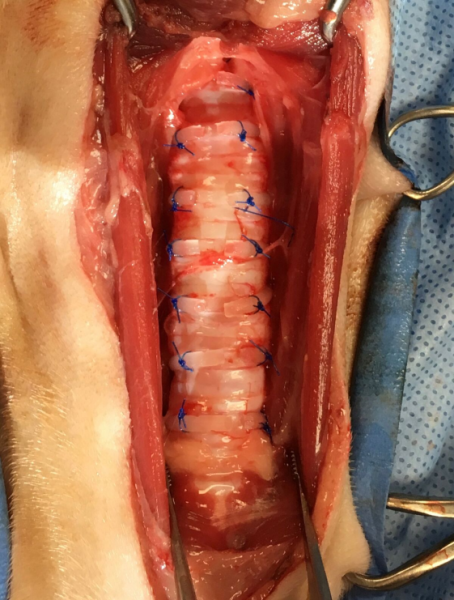
Photos of a trachea with extraluminal tracheal rings in place.
Courtesy of Dr. Joanne Franks, Dallas Veterinary Surgical Center
Tracheal rings can only be placed on the part of the trachea in the neck. Dogs with tracheal collapse inside the chest may not be good candidates for tracheal rings.
Tracheal ring surgery is usually successful, making symptoms less severe. Life-long weight control and medications are still necessary. Potentially serious and life-threatening complications are possible. Over time, tracheal collapse within the chest may worsen, and placement of a tracheal stent may also be necessary.
Possible postoperative complications may include pneumonia, implant failure, peri-tracheal swelling, hemorrhage, tissue necrosis, obstructed breathing, ongoing collapse of the trachea inside the chest, and death. This procedure has a high survival rate as well as a high complication rate so diligent postoperative care is crucial. Clinical signs can resolve as early as two weeks postoperatively and in one study approximately 60% of patients no longer required medical management.
Tracheal Stent Placement:
Intraluminal tracheal stents are used to expand the trachea from the inside out. They are composed of a nickel-titanium alloy and shaped into a hollow cylinder of mesh. The stent is placed with the aid of fluoroscopy, and once positioned correctly the unit is deployed inside the trachea.
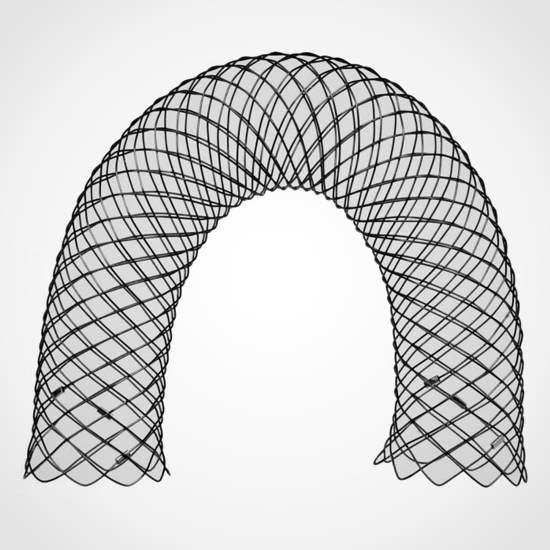

Infiniti Medical vet stent (above) and radiograph of a dog with a stent in place.
Courtesy of Dr. Joanne Franks, Dallas Veterinary Surgical Center
Intraluminal tracheal stents can offer immediate dramatic improvements however they can have potentially serious complications. These stents are placed in an area of high motion and are thus prone to kinking and breaking. The patient may also cough for several weeks since the stent causes irritation in the airway initially before the lining of the airway grown over it. Sometimes the stent can stimulate an over-exuberant growth of tracheal lining over the implant and thus cause a secondary obstruction. Due to these serious complications, intraluminal stenting should
be reserved for patients who have failed medical management and are not good candidates for extraluminal rings.
Tracheal stent placement is usually successful, making symptoms less severe. Life-long weight control and medications are still necessary. Potentially serious and life-threatening complications are possible.
Prognosis and Postoperative Care
The long-term clinical signs of tracheal collapse patients can be extremely variable given the various grades of the disease as well as its progressive nature. Most patients need ongoing medical management following either one of the surgical procedures. There is no cure for tracheal collapse and neither surgery offers a permanent cure. Rather, surgery is a tool for management of tracheal collapse and can increase survival with the disease.
Following surgery, the patient will need to be monitored in hospital for one to two days postoperatively. Antibiotics may be necessary to treat any concurrent respiratory infection. Patients are usually continued antitussive and anti-inflammatory therapies for a month postoperatively. Improvements in clinical signs are usually noted between 2-4 weeks following surgery.
Prognosis varies and can be determined by an experienced veterinary surgeon on a case by case basis.
Search This Site
Medical Library Posts
- 25+ Years of Neurosurgery at the DVSC
- Anal Sac Adenocarcinoma
- Anal Sac Removal, Elective
- Arthritis
- Arthroscopy
- Atlanto-axial (A-A) instability
- Coxofemoral (Hip) Luxation
- Cranial Cruciate Ligament (CCL) Overview
- Cranial Cruciate Ligament (CCL) – Extracapsular Repair
- Cranial Cruciate Ligament (CCL) – Tibial Plateau Leveling Osteotomy (TPLO)
- Cranial Cruciate Ligament (CCL)-Tibial Tuberosity Advancement (TTA)
- Cutaneous Mast Cell Tumors
- Cystotomy and Scrotal Urethrostomy
- Degenerative Myelopathy
- Diaphragmatic Hernia
- Diskospondylitis
- Ear Canal Ablation and Bulla Osteotomy
- Elbow Dysplasia
- Epidural Analgesia
- Episioplasty
- Feline Perineal Urethrostomy
- Femoral Head Ostectomy (FHO)
- Fibrocartilaginous Embolism (FCE)
- Fibrocartilaginous Embolus in Schnauzers
- Fracture Healing by Biologic Osteosynthesis
- Fracture of the Radius and Ulna in Small breed dogs
- Fracture Repair by Circular External Skeletal Fixator (ESF)
- Gastric Dilatation-Volvulus (Bloat)
- Gastrointestinal Foreign Body
- Gastropexy, Elective
- Hip Dysplasia (Overview)
- Hip (Coxofemoral) Luxation
- Incontinence: Urethral Sphincter Mechanism Incompetence
- The Facts About Backs (IVDD)
- Intervertebral Disc Disease (IVDD) Percutaneous Laser Disc Ablation LDA
- Intervertebral Disc Disease (IVDD)- Care of a Paralyzed Pet
- Laryngeal Paralysis
- Lumbosacral Disease
- Mandibulectomy and Maxillectomy
- Medial Patellar Luxation (MPL)
- Microvascular Dysplasia Mimics Portosystemic Shunt
- Minimally Invasive Surgery in Soft Tissue Applications
- Neurosurgical Postoperative Physical Therapy
- Perianal Fistula Management in Dogs
- Perineal Hernias
- Peritoneopercardial Hernias in Dogs and Cats
- Portosystemic Shunts
- Sialocele (Salivary Mucocele)
- Spinal Fractures and Subluxations
- Splenectomy
- Total Hip Replacement
- Tracheal Collapse
- Triple Pelvic Osteotomy (TPO)
- Underwater Treadmill
- Updates in Fracture Management
- Urethral Prolapse
- Wobblers Disease
Comments Closed